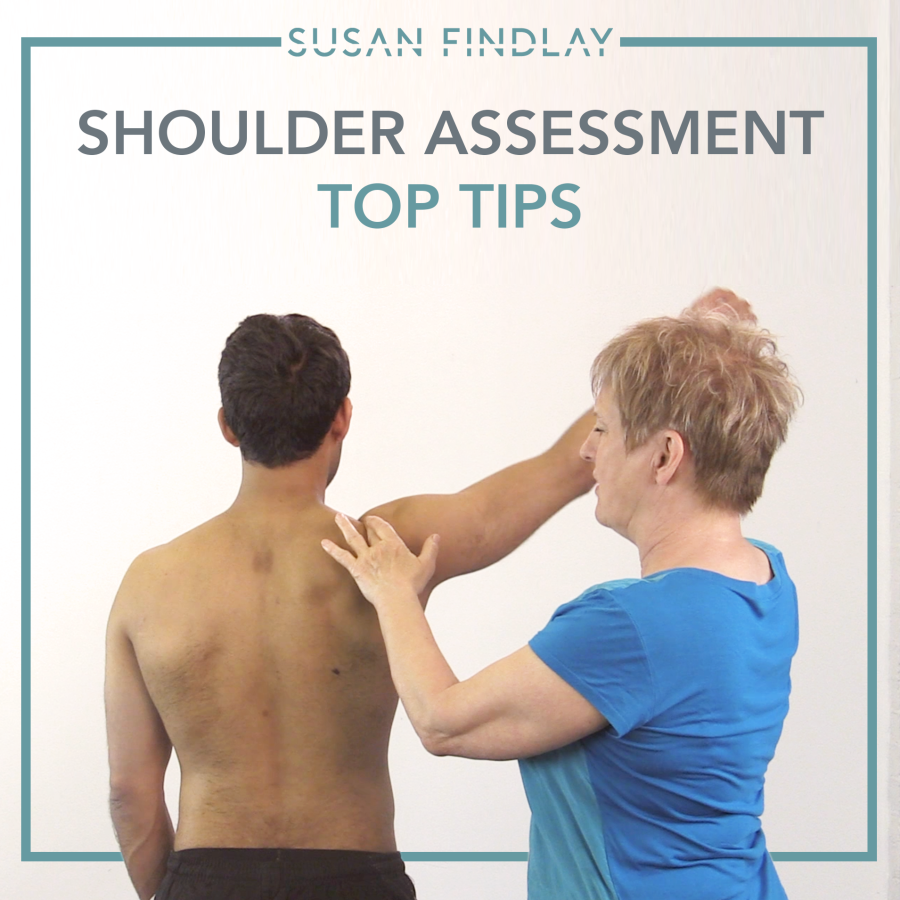
Shoulder issues are common as they are a highly used part of the body which is put under frequent strain. It is also an area of the body that is particularly interconnected with integral joints, such as the neck, ribcage, scapula, clavicle, and spine. All too often clients come to me after being diagnosed with chronic conditions that have been prescribed medication as the long-term treatment option. I find this a highly unfortunate situation as many skeletal and functional issues are either soft tissue conditions that have been misdiagnosed or could be vastly improved with soft tissue therapy. I think most therapists will agree that little can change unless the soft tissue surrounding the area is reorganised and new movement encouraged.
In this blog I will take you through a five part approach when assessing a shoulder.
Part 1 – Meeting the Client
My favourite part of the whole massage process is listening to my clients’ story. Hearing about their lifestyle, job, and activities as well as any operations, accidents, or medical issues. This allows me to gain important information about them as a person, it helps me to determine the basis of their understanding and what their priorities are. This is key to the entire assessment as well as the success of the treatment process.
During the subjective stage I tend to ask for a detailed explanation of their daily habits followed by an example of a functional movement. This gives me a clear idea of their functional movement patterns and habits. It also provides an understanding of the character of the client, as a positive perspective and client cooperation is key to rehabilitation.
Following on from the face-to-face assessment (nowadays I often do my subjective assessment via zoom), I will do a visual check, to be fair, this process started the moment they walked in, I like to do my assessments without them knowing they are being assessed, I look for how they carried themselves, facial expressions, how they sit in a chair, are they fidgeting, etc.
A shoulder assessment can be carried out in any position. Sitting on the bed, supine, prone or standing all have value and will give you needed information. Our behaviour is not based on a linear line, we need to get away from the lever system of biomechanics, we function as a whole in multidimensional planes, I refer to this as a biotensegral mechanics, this involves a whole body integrated approach.
Part 2 – Seated Assessment
 Here, we start with a seated assessment looking at the back of the torso. The arrangement of the back is highly dependent on shoulder placement. The ribs need to be able to move, as does the clavicle, and the scapulae, they need to freely glide. All of these are key components that allow a shoulder to optimally function.
Here, we start with a seated assessment looking at the back of the torso. The arrangement of the back is highly dependent on shoulder placement. The ribs need to be able to move, as does the clavicle, and the scapulae, they need to freely glide. All of these are key components that allow a shoulder to optimally function.
We need to consider the placement of the head and the movement of the neck in relationship to the shoulders. It is helpful to make note of the following: Is the head tilted to one side? Are the ears fairly even? Is the length from neck to tip of shoulder even? Is one shoulder elevated higher than the other? These give you hints to the overall function of the shoulder rather than a diagnosis.
Check the position of the scapulae and their borders, observe the height of the end points (inferior medial borders) from one side to the other, consider if any of the differences are connected to the anterior of the shoulder i.e. protraction or does it come from the ribs or lower torso. It is even possible that an ill-aligned scapula originates from a problem with the feet!
It is key to take note of all of these aspects but refrain from making a diagnosis. Even if an issue looks obvious to you an early diagnosis can come back and bite you, sometimes the answers are not what are readily obvious. For instance, when coming across an injury there is frequently an imbalance of muscle mass which indicates tension in the system, this could be global so always look away from the area of complaint, observe any build ups of tissue globally and check for signs of atrophy or high activity.
I do discuss functional movement in my videos online, these include simple exercises that can evaluate movement, tension, functionality, and pain level.
Part 3 – Standing Assessment
 An evaluation in standing posture can achieve strikingly different results to that of sitting. As the client’s pelvis is activated, we can note anterior tilt, any flatness in the back, curvature of the spine and the position of the head.
An evaluation in standing posture can achieve strikingly different results to that of sitting. As the client’s pelvis is activated, we can note anterior tilt, any flatness in the back, curvature of the spine and the position of the head.
Re-check all the areas from the seated position, comparing any changes, new insights or imbalances. It is worth taking into consideration how they spend the majority of their time, seated at a computer or actively moving all day.
There are multitudes of exercises we can undertake here, such as; lifting the arms, rolling the shoulders, circumduction, abduction, etc. However, you only need to undertake the exercises that are relevant to the complaint. My main job, which I highly value as my number one assessment tool is touch, and through feeling the tissue I can determine which areas I need to explore further. So while a postural, or standing assessment has value it is not my main source of information.
Part 4: Couch Assessment
 Ok, this is where we get to the crux of what we do as soft tissue therapists, I can start my assessment whilst the client is in a supine, but it is not exclusive, I can also do it in all positions.
Ok, this is where we get to the crux of what we do as soft tissue therapists, I can start my assessment whilst the client is in a supine, but it is not exclusive, I can also do it in all positions.
Before you make any adjustments to a clients’ position on the couch, observe how the client naturally lies before you make any form of intervention. Again, compare lengths from neck to shoulder, from neck to clavicle, clavicle to pecs, elevations and head positioning.
The importance of touch really comes into action here as you start palpating, warming and softening the areas, whilst gently checking for resistance and bounce. Before I start to integrate any advanced techniques, I rely on simple approaches that include multidirectional compression, I am looking for rebound movements, comparing both sides, assessing for discomfort, which direction gives ease, this helps to build a picture of functional behaviour that will help me to plan the treatment of the session.
Once I have a good idea of the story, not necessarily the one they told me verbally but the nonverbal one the body is relaying to me, I can start to consider the more advanced techniques and which ones would be useful. At this stage I like to carry out a combination of MET and Transverse STR techniques. MET (Muscle Energy Technique) is where we work to gently contract the muscles to relax, lengthen the muscles and increase joint motion. TSTR (Transverse Soft Tissue Release) is a remedial technique, which aims to return glide and bounce back into the connective tissue (fascia). I often integrate the breath into both techniques as it can be crucial to triggering internal dynamics and create movement as well as relaxation. It is what I refer to as internal massage.
I will use a combination of techniques that aim to create space and encourage the body to initiate its own movement. I believe that we are facilitators, we encourage change, but the body does the majority of the work after the session.
The application of treatment is not trying to achieve symmetry, rather my objectives and the direction my decisions from which my treatment is based on is reliant on what I palpate rather than what I see. Touch is far more accurate for me as a massage therapist than visual or functional methods. Hence, my session outcome is not based on visual symmetry but how to create movement that is both stable and functions with ease.
Part 5: Homecare
 Homecare is an essential part of treatment and the client needs to prioritise it. It is essential therefore that it does not feel like a burden or a chore to the client but instead something to look forward to.
Homecare is an essential part of treatment and the client needs to prioritise it. It is essential therefore that it does not feel like a burden or a chore to the client but instead something to look forward to.
From the notes made in Part 1 you will have an idea how your client can integrate homecare seamlessly into their day, as well as how to make it fun or appealing.
I tend to only give short, simple exercises that are proprioceptive. Subtle exercises like these tell us which muscles are driving the movement as well as reorienting the messages from the brain to muscle. Proprioception is the body’s ability to sense its location, movements, and actions, and all too often in a physical complaint like the shoulder, we can note that the brain has stopped sending the right messages to the right muscles.
Clients are often looking for a ‘quick fix’ but before any strengthening or power work can be undertaken it is essential to improve core movement and function in simple, small ways that are manageable, and clients can undertake on a daily basis.
So, the rule of thumb is when you create more movement in one area, stability is needed in another, therefore I would propose that you allow the body to adapt to its new movement patterns before introducing an extreme change. Less is more, especially when working with soft tissue.
Please feel free to join in the online shoulder workshop which goes through this in greater detail.